Cervical Cancer
 Cervical cancer develops through pre-cancerous stages over many years and usually has no symptoms. The National Cervical Screening Program detects the human papillomavirus (HPV), a common infection and the cause of almost all cervical cancers. Combined with the HPV vaccination program, finding and treating pre-cancerous cervical cell changes will prevent them developing into cancer.
Cervical cancer develops through pre-cancerous stages over many years and usually has no symptoms. The National Cervical Screening Program detects the human papillomavirus (HPV), a common infection and the cause of almost all cervical cancers. Combined with the HPV vaccination program, finding and treating pre-cancerous cervical cell changes will prevent them developing into cancer.
- An estimated 946 women will be diagnosed with cervical cancer in Australia in 2025;
- Cervical cancer is the fourteenth most commonly diagnosed cancer among females in Australia;
- Approximately 254 women will die from cervical cancer in 2025;
- The 5-year survival rate (2017-2021) for ovarian cancer is about 76.8%.
Data sourced from the Australian Institute of Health and Welfare.
Symptoms
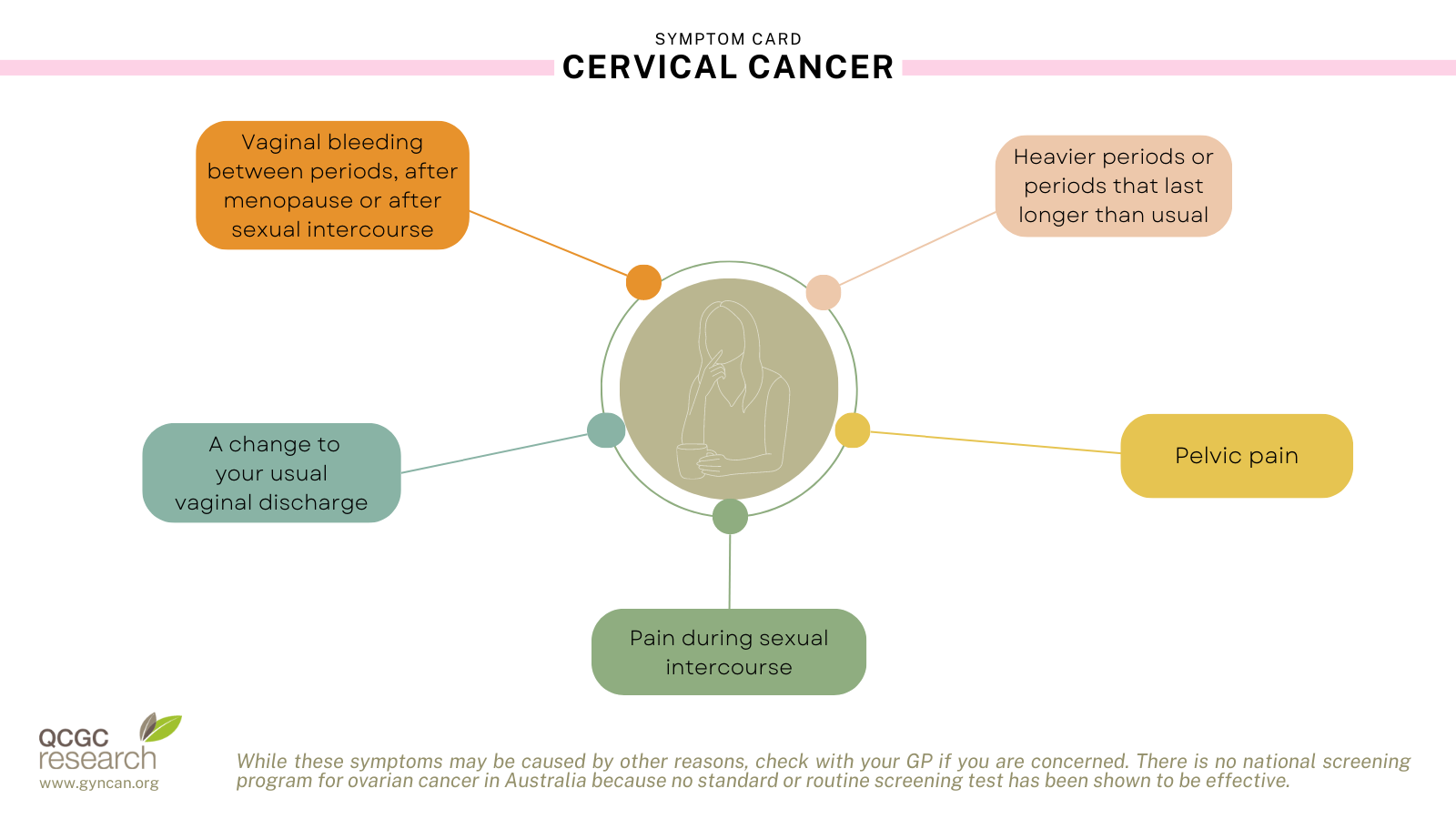
Advanced cervical cancer is very uncommon, but it may cause:
- extreme tiredness
- leg pain or swelling
- lower back pain.
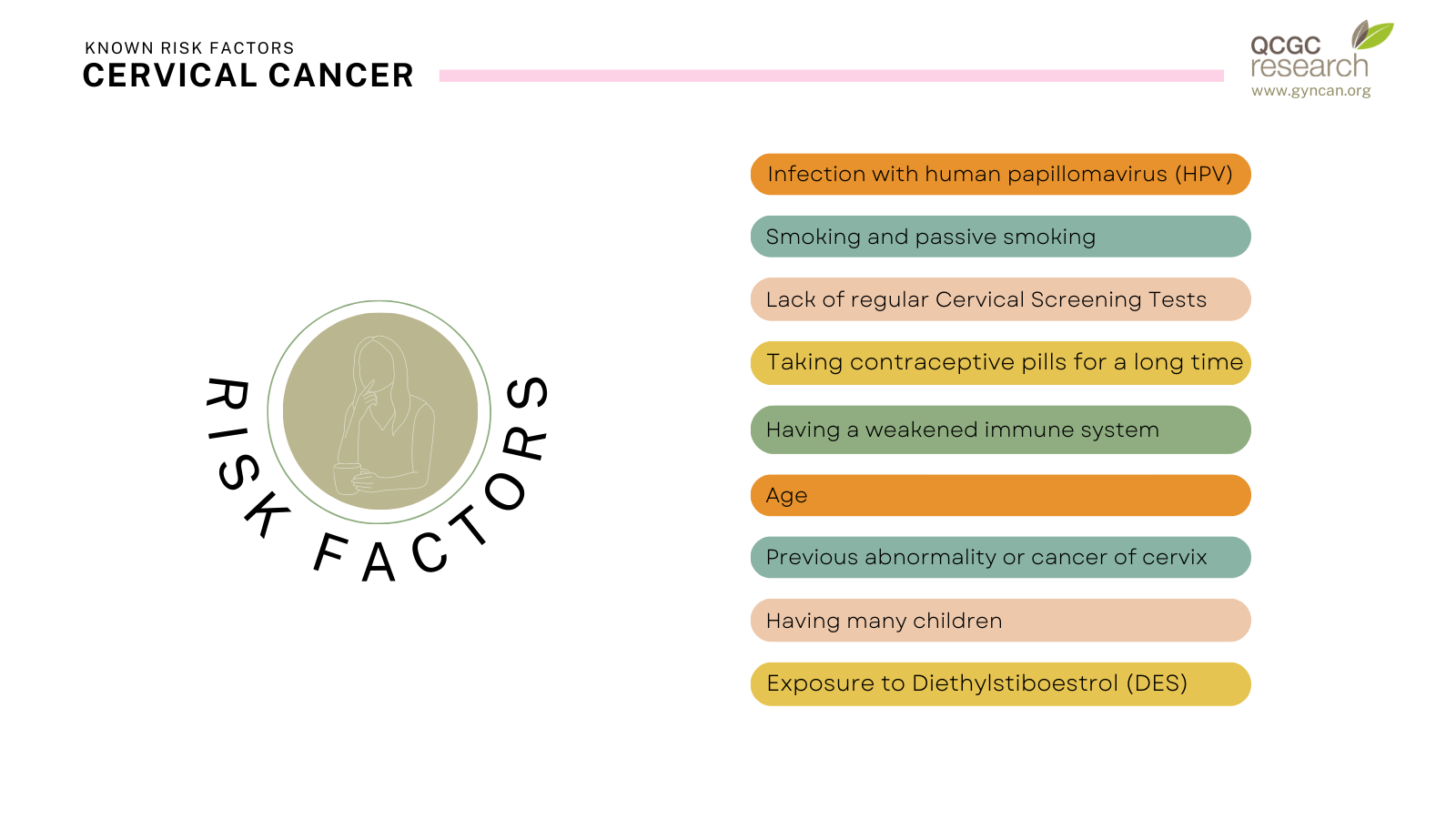
Known risk factors
Prevention and Screening
The HPV vaccine can help prevent cervical cancer. The HPV vaccine protects against infection with some types of HPV, which are the major cause of cervical cancer. HPV vaccine is most effective when it’s given to young people before they become sexually active. Girls and boys aged 12–13 can receive the HPV vaccine for free under the National Immunisation Program at their school.
Screening is the use of tests to detect a disease in people who have no symptoms. You should start testing at age 25, but it’s never too late to start. Following your first Cervical Screening Test, you should screen every 5 years until age 70-74. After this age, the risk of developing cervical cancer is very low and you can usually stop cervical screening.
Around eight out of 10 women will become infected with genital HPV at some time in their lives. Most women who have the HPV infection never get cervical cancer; only a few types of the HPV result in cervical cancer.
Diagnosis and Treatment
Treatment depends on the stage of disease. Very early cervical cancer (microinvasive) can be treated by a cone biopsy or a simple hysterectomy. Patients with cervical cancer limited to the uterine cervix require a radical hysterectomy, at which a safety margin around the cancer is taken. These patients also require removal of lymph nodes along the large blood vessels in the pelvis. Patients with advanced disease (stage 2+) require a combination of chemotherapy (weekly) plus radiotherapy (daily) for four to six weeks. Survival depends on the stage of disease with more than 75% of patients surviving stage 1.
See the Cancer Australia website for more information on diagnosis testing and treatment options.
Source: Cancer Australia; Cancer Council
