NODE Study
Vulvar cancer develops from the skin of the vulva. It can spread locally to nearby structures (such as the vagina, urethra, and anus) or through lymphatic channels to the lymph nodes in the groin. Lymph nodes are a key part of the immune system, filtering harmful substances, including cancer cells, from the body and helping fight infections.
The standard treatment for vulvar cancer involves surgery to remove the primary tumour and, if needed, the groin lymph nodes — a procedure known as lymph node dissection. This can be done via a full dissection, where all the groin nodes are removed, or a sentinel node biopsy (SNB), where only one or two selected nodes are removed.
While lymph node dissection is often curative, it is associated with significant short- and long-term complications. These include infections, blood buildup (hematoma), fluid buildup (seroma), pain, swelling (oedema), and reduced mobility. A more serious complication is lymphedema, where the legs, genitals, and surrounding areas experience chronic swelling. Some patients may also suffer from persistent pain, nerve damage, or difficulty performing everyday activities.
Despite being a rare cancer, at least 2500 survivors of vulvar cancer live in Australia.
Most survivors live with detrimental, life-long side effects of their cancer treatment because there are currently no alternatives to mitigate these impacts.
We propose to reduce surgical morbidity by replacing upfront groin lymph node dissection for vulvar cancer patients with serial high-resolution ultrasound monitoring to detect groin metastases. Groin lymph node dissection will only be required for the few women with ultrasound-detected metastases when they are still small.
The NODE trial aims to determine the feasibility of randomising stage IB and II vulvar cancer patients to either (1) non-invasive, serial, high-resolution bilateral groin ultrasound monitoring in conjunction with clinical examination every 2 months, or (2) upfront surgical groin node dissection (performed through either sentinel node biopsy or inguinofemoral lymph node dissection).
If the trial demonstrates feasibility, we will proceed to a phase III randomised clinical trial.
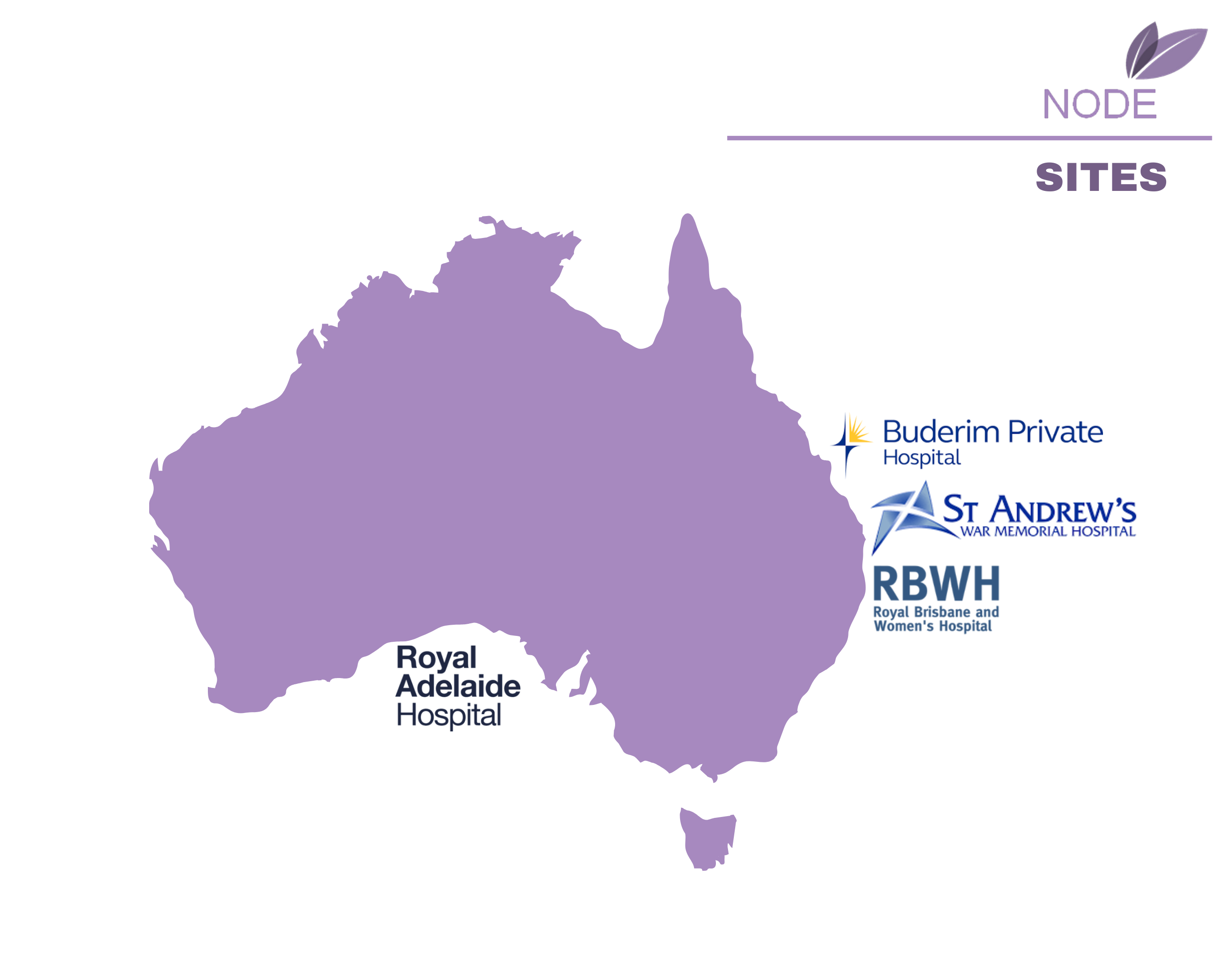
Trial Sites
Recruitment
The NODE trial opened for recruitment in July 2024.
The study aims to recruit 30 participants from national sites. 5 participants have been enrolled to date.
Contact Us
For further information please contact the vulvar cancer clinical trial team at anvutrial@uq.edu.au.
Trial Registration: NCT06264167
