Pre-ANVU Cohort Study
Study 1: Feasibility Of Groin Ultrasound to Predict Groin Lymph Node Involvement in Patients with Histologically Proven Vulvar Cancer
Vulvar cancer is a rare disease that, by its intimate nature, is also largely hidden from public discourse. Approximately 400 Australian women are diagnosed every year, and an estimated 2,500 Australian women currently live with the detrimental effects of vulvar cancer treatment.
Standard treatment of vulvar cancer includes surgery to remove the primary tumour plus the removal of groin lymph nodes. While this treatment is often curative, the removal of groin lymph nodes is associated with debilitating long-term outcomes, including painful and disfiguring limb swelling (lymphoedema), compromised function, impaired mobility, and greater susceptibility to infection for virtually all women.
Women with vulvar cancer know and fear the outcomes of groin lymph node removal and describe life after this procedure as traumatic.
The aim of Pre-ANVU Study 1 is to assess whether non-invasive groin ultrasound is a feasible and accurate method of predicting groin lymph node involvement (i.e. the presence of cancer in groin lymph nodes) in vulvar cancer patients.
The ability to predict the absence of groin node involvement by ultrasound may spare future vulvar cancer patients from the unnecessary removal of groin lymph nodes, thereby reducing complications, improving recovery time, and facilitating their return to normal daily activities.
If the study demonstrates feasibility and accuracy of groin ultrasound to predict groin lymph node involvement, we will proceed to a phase III randomised clinical trial.
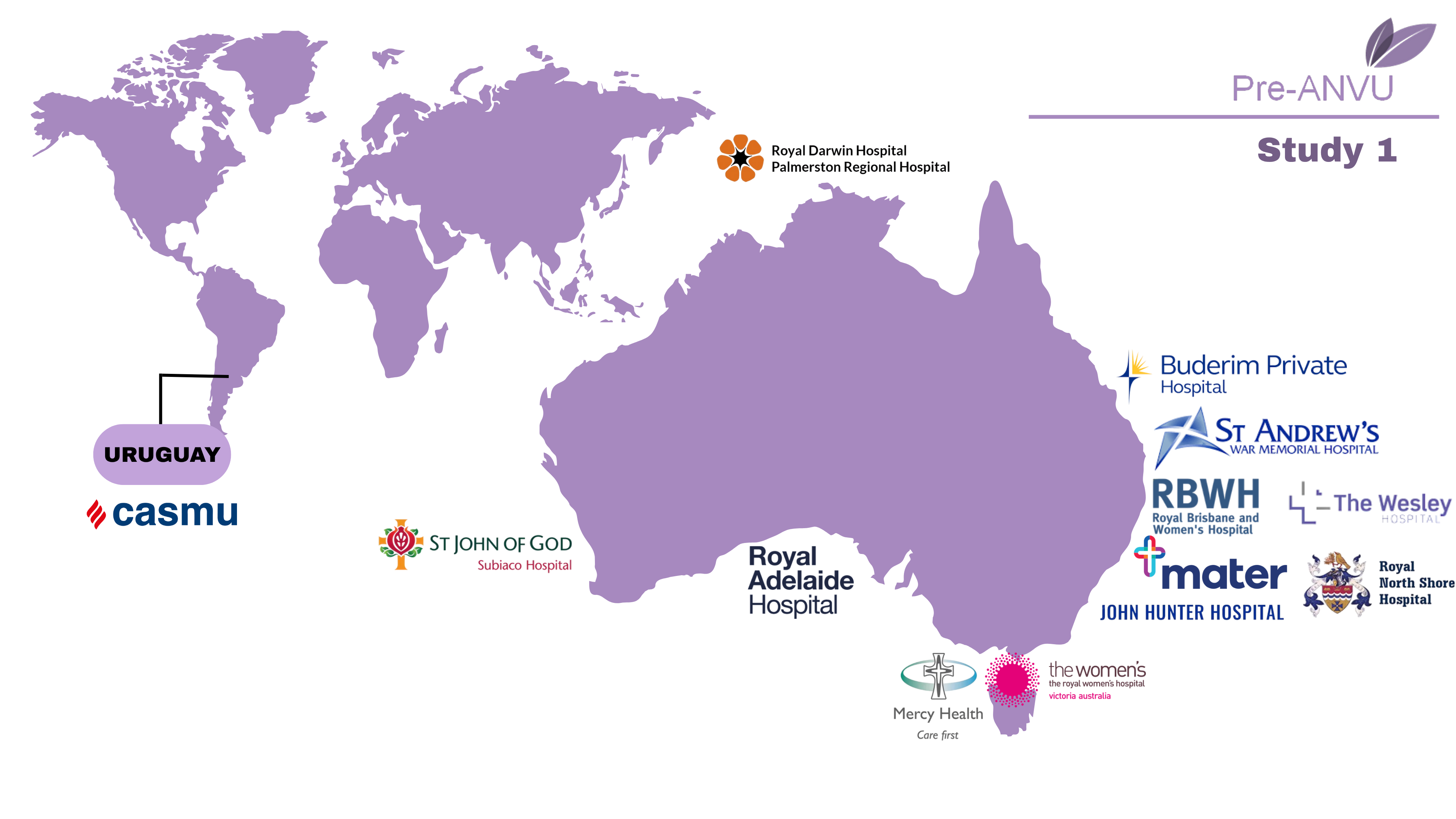
Trial Sites
Recruitment
The Pre-ANVU trial opened for recruitment in August 2022.
The study aims to recruit 65 participants from national and international sites. 52 participants have been enrolled to date.
Study 2: Feasibility Of Biomarker Discovery in the Differential Diagnosis of Vulvar Intraepithelial Neoplasia (VIN) Versus Invasive Vulvar Cancer
Vulvar cancer develops through its precursor lesion, called vulvar intraepithelial neoplasia (VIN).
The incidence of VIN has increased over recent decades and is approximately one per 100,000 women, with a peak occurrence in women aged 30-49 years.
VIN can be classified into grades 1, 2, or 3. VIN2 and VIN3 (high-grade VIN) are direct precursors to vulvar cancer which, if left untreated, will lead to invasive cancer. Diagnosis of high-grade VIN is through a punch biopsy and histopathological assessment. Current standard treatment involves a wide local excision of the involved skin and surgeons aim to achieve negative margins to reduce the risk of local relapse.
Occasionally, a patient receives a biopsy result suggestive of VIN, but final histopathological assessment of the wide local excision specimen subsequently reveals a diagnosis of invasive vulvar cancer. These unwanted situations occur through sampling error, which to some extent is unavoidable. In such a case, if the cancer is stage as IB or higher, the patient will require an additional surgical procedure (groin lymph node dissection).
Study 2 will demonstrate the feasibility of collecting biospecimens from patients and identifying biomarkers of clinical relevance that may be used to accurately differentiate between VIN and invasive vulvar cancer.
Trial Sites
Recruitment
The study aims to recruit 30 participants from Queensland, Australia. Enrolment is now complete.
Contact Us
For further information please contact the vulvar cancer clinical trial team at anvutrial@uq.edu.au.
Trial Registration: ACTRN12622000886785

