TUBA-WISP II Study
QCGC Research is proud to partner with the Radboud University Medical Center, Netherlands, on the TUBA-WISP II Study.
The TUBA-WISP II study aims to determine whether removing the fallopian tubes while delaying the removal of the ovaries is as effective in preventing ovarian cancer as removing both the tubes and ovaries at the same time. This study focuses on women at high risk of ovarian cancer due to an inherited gene variant (BRCA1, BRCA2, BRIP1, RAD51C, RAD51D and PALB2). The research seeks to answer whether this alternative approach is equivalent to the standard method in preventing ovarian cancer for women with these genetic risks, without the short-term symptoms and long-term health risks.
Ovarian cancer can affect the ovaries, fallopian tubes, and peritoneum (the lining of the abdomen). Unfortunately, it is often diagnosed at an advanced stage, and around half of the patients with advanced-stage ovarian cancer die within five years despite treatment.
When ovarian cancer is detected early, most patients survive.
Women in the general population have a less than 1% (1 in 100) lifetime risk of developing ovarian cancer. In contrast, those with BRCA1 or BRCA2 gene variants have up to a 44% (44 in 100) lifetime risk. Carriers of BRIP1, RAD51C, or RAD51D gene variants have an increased risk of ovarian cancer, estimated at 5% to 13%. The lifetime risk for ovarian cancer with a PALB2 PV ranges from 3-5% and a risk-reducing surgery can be considered when the lifetime risk is >5%.
For women with these gene variants, the standard preventive approach is to remove both the ovaries and fallopian tubes, significantly reducing the risk of ovarian cancer. However, this procedure causes immediate menopause, which can lead to short-term symptoms and long-term health risks. Removing only the fallopian tubes does not trigger menopause, offering a potential alternative for risk reduction.
Research suggests that the most common form of ovarian cancer may originate in the fallopian tubes, leading to the hypothesis that removing just the tubes might be sufficient to reduce ovarian cancer risk. The TUBA-WISP II study is designed to compare this alternative method (removal of the tubes with delayed ovary removal) to the standard method (removal of both tubes and ovaries at the same time) in a large clinical trial.
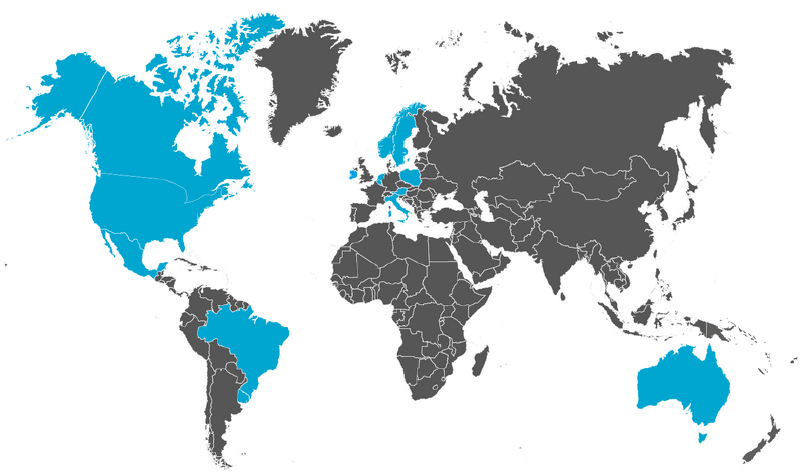
Trial Sites
Recruitment
The TUBA WISP II Study opened for recruitment in March 2020.
The study aims to recruit 3000 participants from international sites. 2000 participants have been enrolled to date.
Eligible participants for the study must have tested positive for an inherited variant in one of the genes that increases their risk of ovarian cancer, including BRCA1, BRCA2, BRIP1, RAD51C, RAD51D and PALB2.
This study is patient-preference based, allowing participants to choose between the standard method (removal of the ovaries and fallopian tubes in one operation) or the alternative method (removal of the fallopian tubes first, with delayed removal of the ovaries at least two years later). The timing of the surgeries may depend on the specific genetic variant a participant carries. The study will compare outcomes between the two groups to determine whether one method is more effective than the other.
Contact Us
For further information please contact the TUBA-WISP II clinical trial team at tuba-wisp@radboudumc.nl or visit the TUBA WISP II website.
Or contact the team here in Australia at qcgcresearch@uq.edu.au.
Trial Registration: NCT04294927
