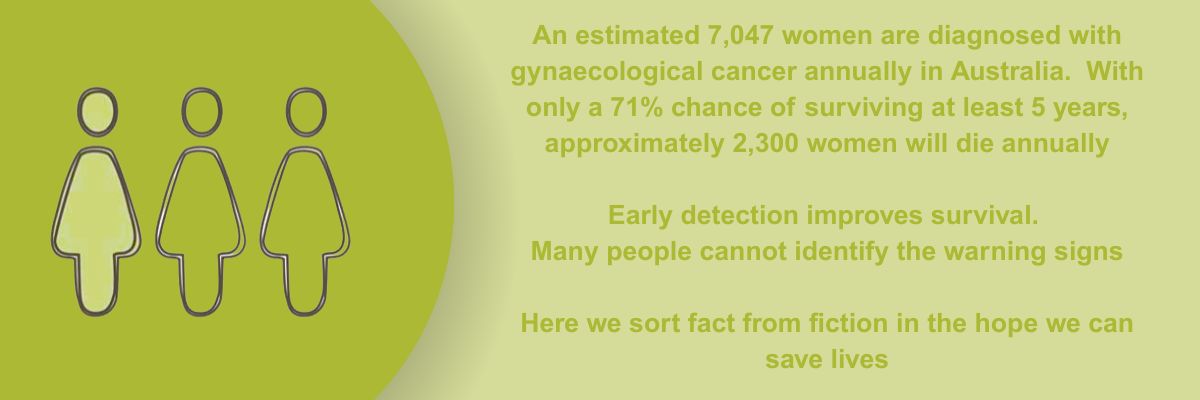
Myths about gynaecological cancer
Gynaecological Cancer ... unravelling the myths!
There are common misconceptions when it comes to gynaecological cancer “facts”. Take a moment to review the following misconceptions as it could save your life!
I have no family history of cancer, so I probably won't get it
Not true. In fact, most women diagnosed with gynaecological cancer have no family history (6 out of 7 for ovarian cancer). Again, the best thing you can do is to closely monitor your body for changes. Survival rates for gynaecological cancer are much higher when women seek medical attention as early as possible.
If I lead a healthy lifestyle, could I still get cancer?
Yes. While we do know that obesity and adverse lifestyle factors such as smoking are directly linked to gynaecological cancers like endometrial cancer, there is no proven 'diet' that prevents cancer. A healthy diet lowers your risk of being diagnosed, but we don't know exactly which foods may fight or prevent cancer. Our advice is to maintain a balanced, healthy lifestyle and avoid risk factors like obesity and smoking that are known to be linked with gynaecological cancer.
Really!? Women who've had a hysterectomy can STILL get gynaecological cancer?
It's true. Not all patients choose to have their ovaries and/or fallopian tubes removed when undergoing hysterectomies. In fact, there have even been rare cases where women with no ovaries were diagnosed with ovarian cancer. Medical professionals are not certain as to why this occurs, but women have been reported as having cancerous cells where their ovaries once were. Some doctors believe that when removed, the ovaries may have already had amounts of cancer so small they were undetectable, leaving traces of cancer cells that subsequently grew in the place of the ovaries. This type of cancer has also presented as 'peritoneal' cancer, which is the thin lining of the stomach. However, biopsies showed the cancer originated from the ovaries (although no longer there).
Recent evidence suggests that the fallopian tubes should be removed during a hysterectomy (even in young women) because it reduces the risk of gynaecological cancer (see TUBA-WISP II Study for more information). Vaginal or vulval cancer is also not avoided through having a hysterectomy.
Does NCSP detect all types of cancer?
No. The National Cervical Screening Program (NCSP) aims to reduce the impact of cervical cancer through the detection of the HPV Virus which can lead to cell changes in the cervix. Our advice is, do not think you are 'safe' from gynaecological cancer because you had a cervical screening test. Be vigilant and if you notice any unusual changes in your body, seek medical advice promptly. If you are unsure, check the government webpage on Who should get a Cervical Screening Test.
But doesn't having multiple sexual partners increase your risk of gynaecological cancer?
You may have read that 'multiple sexual partners' increase the risk of gynaecological cancer. This is often misconstrued to mean that sexual promiscuity in itself is a risk factor and in the past, has caused society to view gynaecological cancer as a 'taboo' topic. Sexual contact with just one person can result in HPV being contracted, so mathematically, having multiple partners simply increases that chance. Contracting cervical cancer does NOT mean that a woman has indeed had many sexual partners.
Over 50% of the population is infected with the Human Papilloma Virus (HPV). Not all types of HPV are dangerous. HPV often goes unnoticed as there are no symptoms. However, certain types of HPV have been linked to the development of cervical cancer.
Do more women die from ovarian cancer than breast cancer?
No, but only because breast cancer is more common. An estimated 1,929 new cases of ovarian cancer are diagnosed, with an estimated 1,064 deaths annually (AIHW 2025 data) compared to an estimated 20,336 new cases of breast cancer diagnosed, and an estimated 3,353 deaths annually. However, women diagnosed with breast cancer have an average 92.7% five year survival rate, compared with just 48.9% five year survival rate for those diagnosed with ovarian cancer (and 70.8% for all gynaecological cancers, Based on AIHW 2017-2021 data).