Ovarian Cancer
 Ovarian cancer is a malignant turmour and occurs when abnormal cells in the ovary, fallopian tube or peritoneum grow in an uncontrolled way. While there are many types of ovarian cancer the three most common types of ovarian cancer are: the common epithelial type (90% of cases) that arises from the cells on the outside of the ovary; the germ cell type (around 4% of cases) that arises from the cells which produce eggs; and the rare stromal type arising from supporting tissues within the ovary.
Ovarian cancer is a malignant turmour and occurs when abnormal cells in the ovary, fallopian tube or peritoneum grow in an uncontrolled way. While there are many types of ovarian cancer the three most common types of ovarian cancer are: the common epithelial type (90% of cases) that arises from the cells on the outside of the ovary; the germ cell type (around 4% of cases) that arises from the cells which produce eggs; and the rare stromal type arising from supporting tissues within the ovary.
Ovarian cancer has been called a “silent killer”, because it typically causes few early symptoms and is usually not discovered until it has spread around the pelvis and abdomen.
- An estimated 1,929 women will be diagnosed with ovarian cancer in Australia in 2025;
- Ovarian cancer is the ninth most commonly diagnosed cancer among females in Australia;
- Approximately 1,064 women will die from ovarian cancer in 2025;
- The 5-year survival rate (2017-2021) for ovarian cancer is about 48.5%.
Data sourced from the Australian Institute of Health and Welfare.
Symptoms
There are often no obvious signs of ovarian cancer, however you may have one or more of the following symptoms:
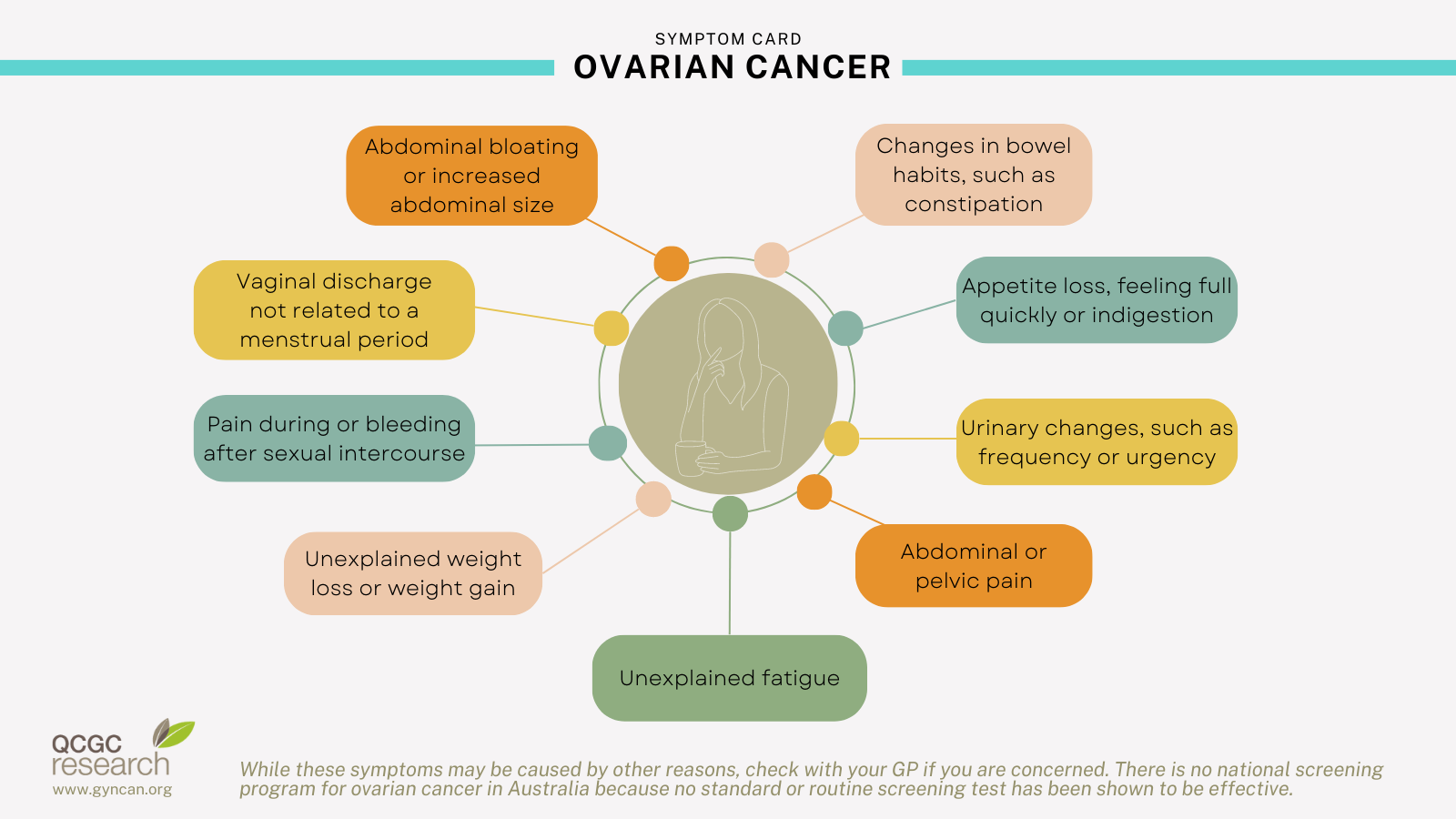
These symptoms do not necessarily mean you have cancer – they might be caused by another health condition.
If you have these symptoms and they are new for you, are severe or continue for more than a few weeks, it is best to arrange a check-up. Keep a record of how often the symptoms occur and make an appointment to see your general practitioner (GP).
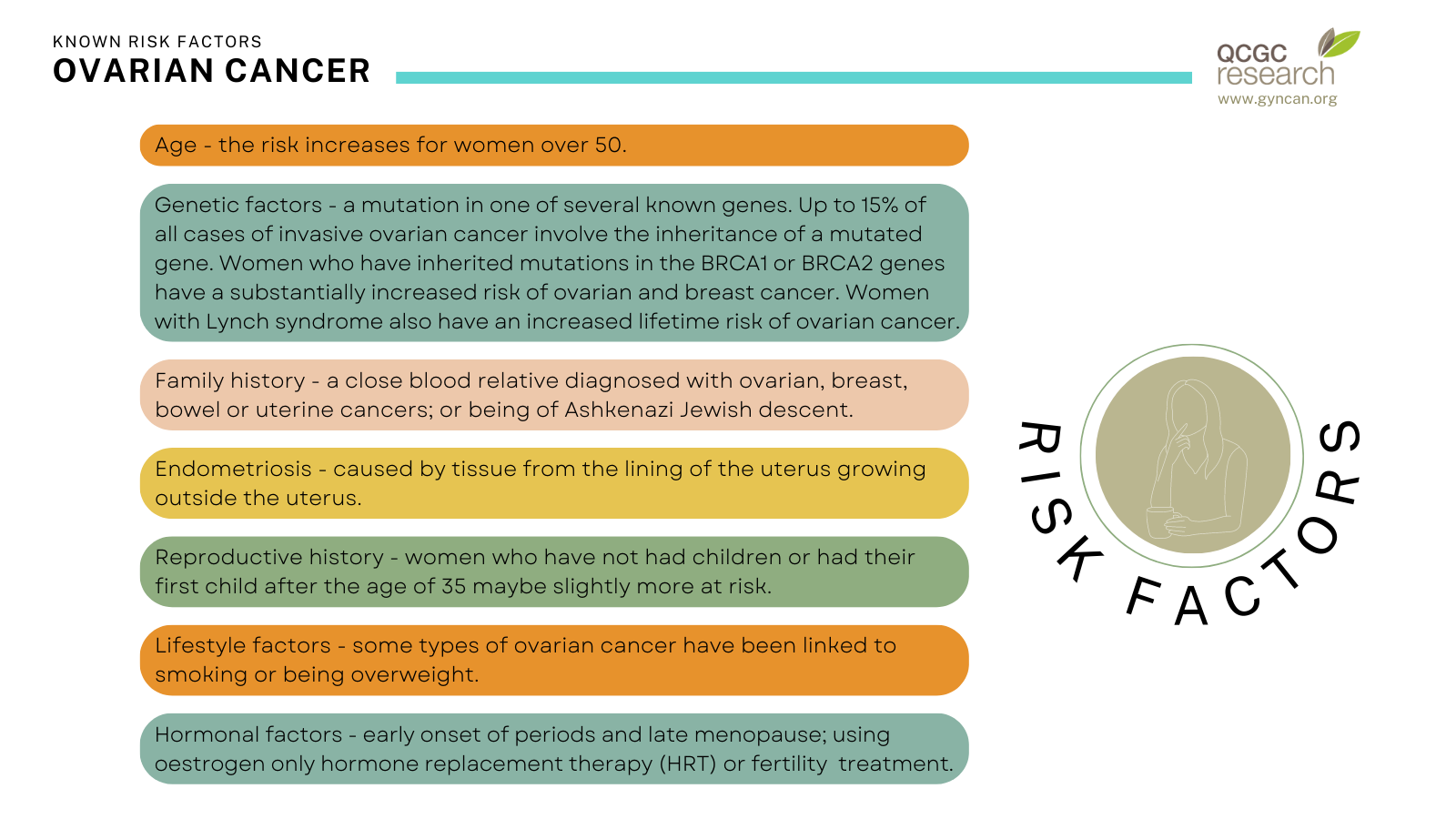
Known risk factors
Factors that are associated with a higher risk of developing ovarian cancer include:
Some factors that may reduce the risk of developing ovarian cancer include using the oral contraceptive pill for several years, having your fallopian tubes tied (or removed), having children before the age of 35 and breastfeeding.
Screening
Currently there are no tests effective enough for a population-based screening program for ovarian cancer.
Know the symptoms and know your body. If you experience any of the symptoms, especially if htey are unusual for you or persistent, it's important to see your doctor.
Diagnosis and Treatment
Due to the lack of early symptoms and inefficiency of screening, two out of three patients are diagnosed at advanced stages (stage three or four).
See the Cancer Australia website for more information on diagnosis testing and stages.
Patients with early stage disease (stage one or two) require surgical removal of the tubes and the ovaries, as well as a staging procedure to determine the extent of cancer spread. Patients with advanced stage ovarian cancer require surgical removal of as much cancer as possible. This may include removal of uterus, tubes, ovaries, omentum, bowel, spleen, diaphragm and abdominal peritoneum. The size of the tumour left behind after surgery determines the prognosis to a large extent. If large scale surgery is not feasible, patients will have some chemotherapy upfront, followed by delayed surgery and more chemotherapy thereafter. Virtually all patients require chemotherapy, to which 85% of patients respond well. However, the majority of patients with advanced ovarian cancer will relapse.
See the Cancer Australia website for more information on treatment options.
The Cancer Council also provides a "Ovarian Cancer: Your guide to best cancer care" which explains the standard of high-quality cancer care that all Australians can expect, from diagnosis, to treatment, recovery, and living with cancer.
Research
Current research focuses on the development of new markers indicating the earliest possible stage of ovarian cancer. Diagnosing and commencing treatment of ovarian cancer early to increase the chance of survival outcomes. Other research addresses the selection of patients for advanced surgery as well as measures to improve recovery from treatment.
Click through to see more information on our ovarian cancer research:
Source: Cancer Australia