Vulvar Cancer
 Vulvar (or vulval) cancer occurs when abnormal cells in the tissues of the vulva grow in an uncontrolled way. About 1,423 Australian women currently live with vulval cancer. It most commonly affects women who have gone through menopause, however vulval cancer can also occur in younger women.
Vulvar (or vulval) cancer occurs when abnormal cells in the tissues of the vulva grow in an uncontrolled way. About 1,423 Australian women currently live with vulval cancer. It most commonly affects women who have gone through menopause, however vulval cancer can also occur in younger women.
- An estimated 401 women will be diagnosed with vulvar cancer in Australia in 2025;
- Approximately 115 women will die from vulvar cancer in 2025;
- The 5-year survival rate (2017-2021) for vulvar cancer is about 74.5%.
Data sourced from the Australian Institute of Health and Welfare.
Breaking the silence - Read Nicola's story.
Symptoms
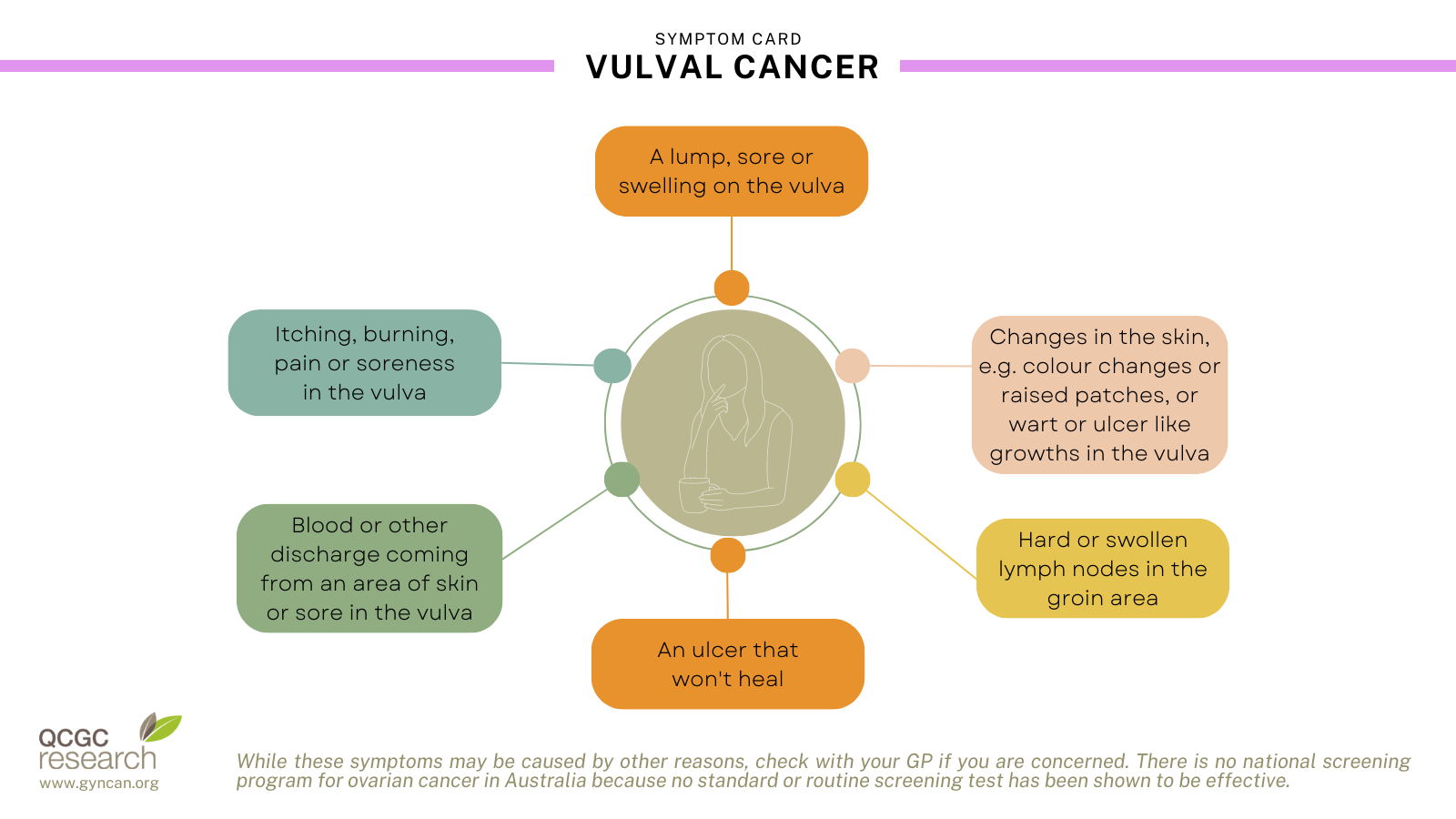
As a precaution, consult your doctor if you experience any of these symptoms.
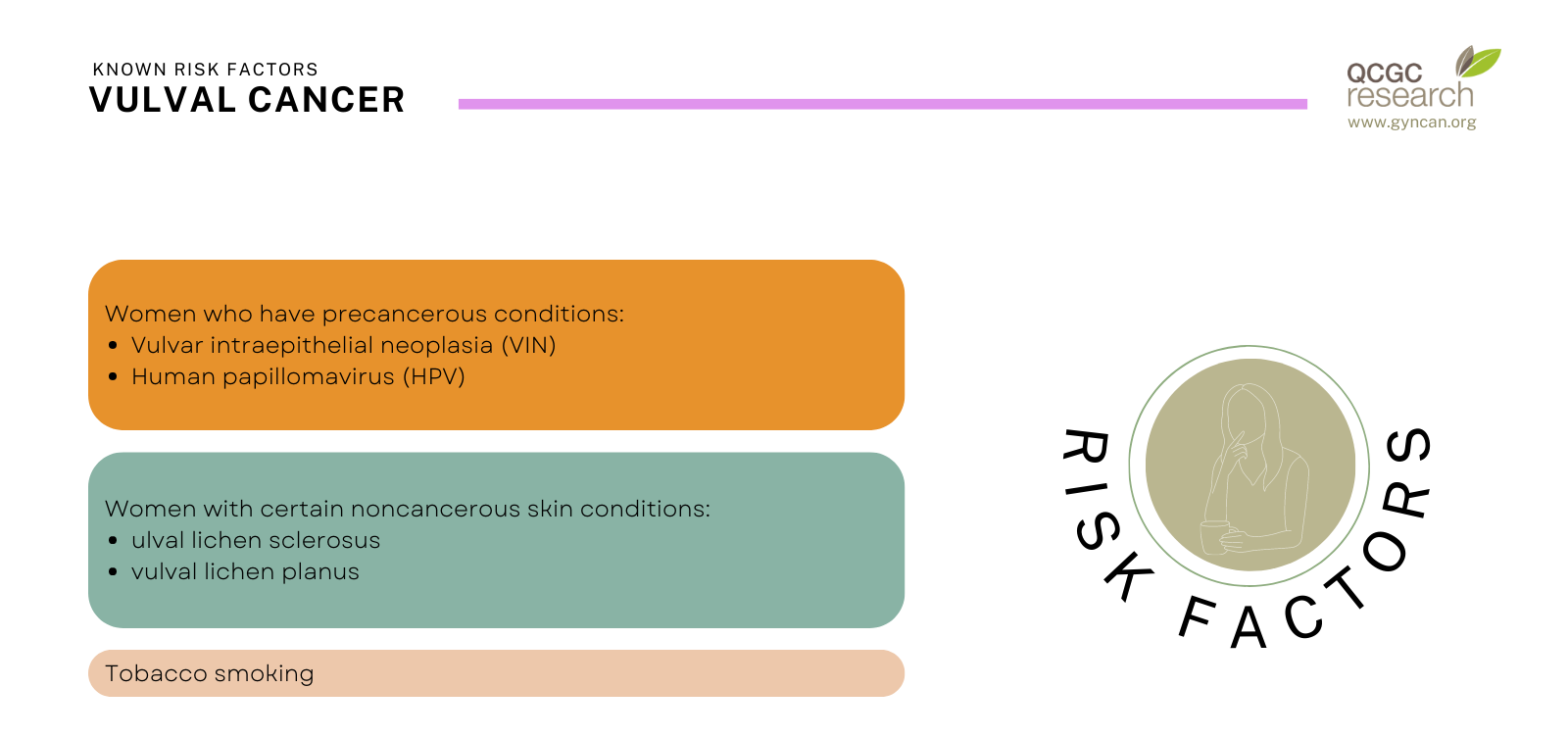
Known risk factors
Screening
There is currently no national screening program for vulvar cancer available in Australia.
Diagnosis and Treatment
The main tests used to diagnose vulvar cancer are a physical examination, a colposcopy, and a tissue biopsy. These tests are usually performed at the same time. Because vulvar cancer is sometimes associated with cervical cancer, the doctor may also check for abnormal cells in your vagina and cervix.
Surgical removal of the involved vulval skin is the main treatment for vulvar cancer. Vulval cancer may spread to the lymph nodes in the groin and therefore they need surgical exploration as well. Selected patients require radiotherapy to the vulva, the groin or both. Survival of vulval cancer is generally good, but the side effects from treatment are significant (wound break down, lymphoedema).
See the Cancer Australia website for more information on diagnosis testing and stages, and treatment options.
Research
Current research focuses on new techniques to determine the spread of the cancer to the lymph nodes rather than removing the lymph nodes initially. The secondary outcomes of surgical removal of lymph nodes can be debilitating, life-long lymphoedema for which there is no cure, it is a chronic and permanent swelling of one or more body parts. Our research aims to reduce the removal of lymph nodes in patients who do not require this proceedure, and reduce the incidence of lymphoedema.
Click through to see more information on our vulvar cancer research:
Source: Cancer Australia